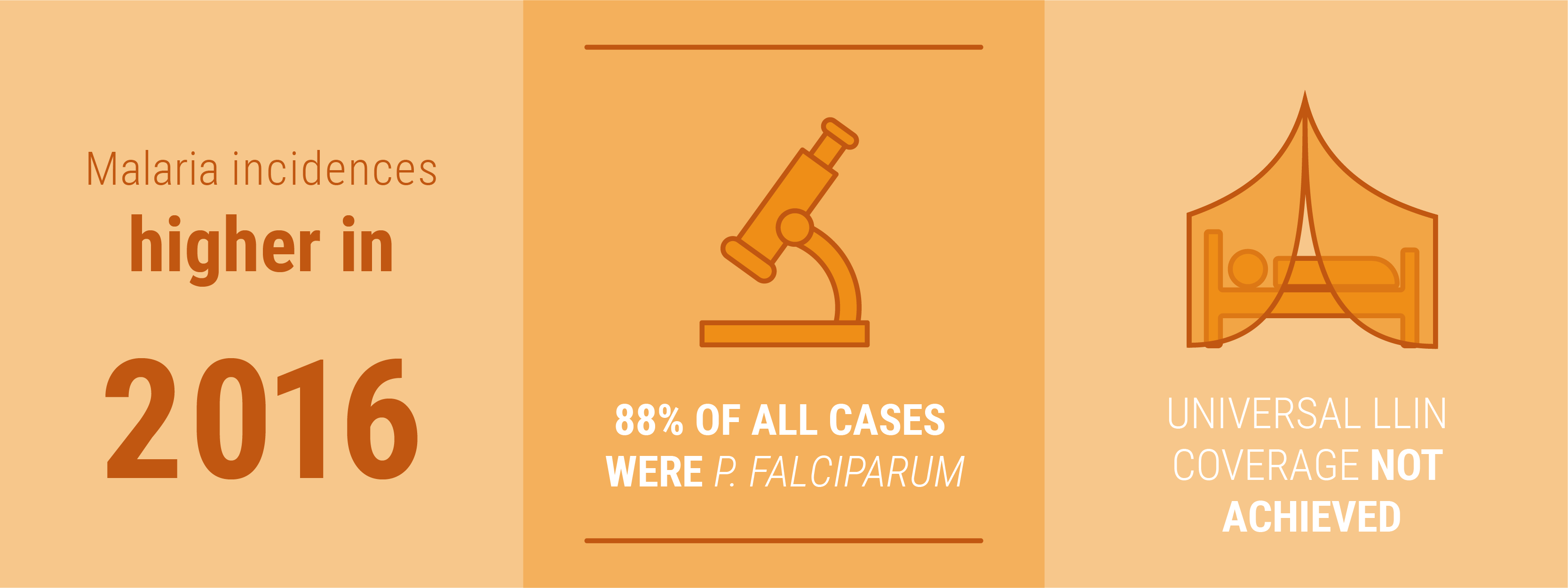
Universal LLIN coverage has not been achieved
Ongoing malaria transmission is the malaria transmission that remains after universal coverage of long-lasting insecticidal nets (LLINs) has been achieved. This study showed that universal coverage of LLINs has not been achieved in the study sites, and therefore not all of the malaria cases seen could be attributed to ongoing malaria transmission.
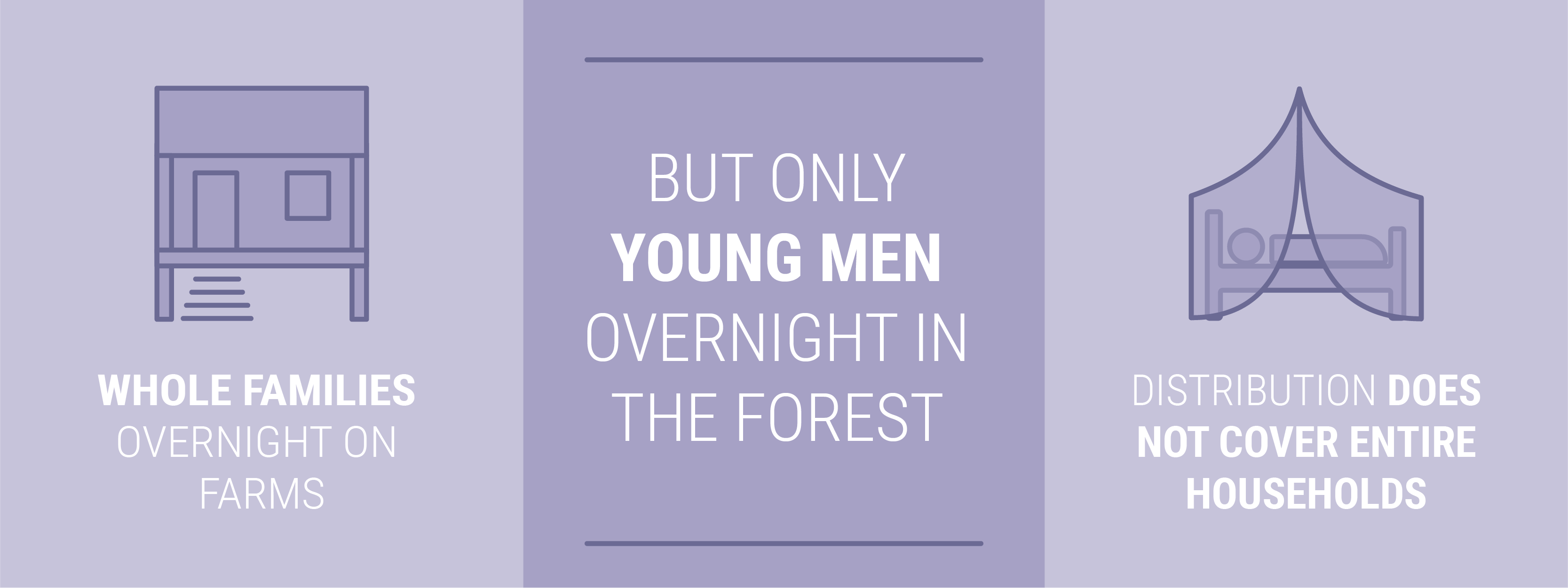
Not enough LLINs had been distributed to cover each family member, and the LLINs provided were not sized for family beds.
LLINs were unavailable in the village markets, and concerns existed about the impregnation of nets with insecticides.
Substandard net maintenance and treatment was prevalent, and villagers used damaged nets.
There was limited to no use of mosquito nets in farm and forest sites. This was because families did not have spare nets to take to their farm huts, nets were cumbersome to carry, or it was not possible to use nets in the farm and forest environments.
Factors contributing to malaria transmission
This study also showed that even if every individual in the study site were to use an LLIN when asleep, malaria transmission could still occur. This was due to a number of reasons, most notably:
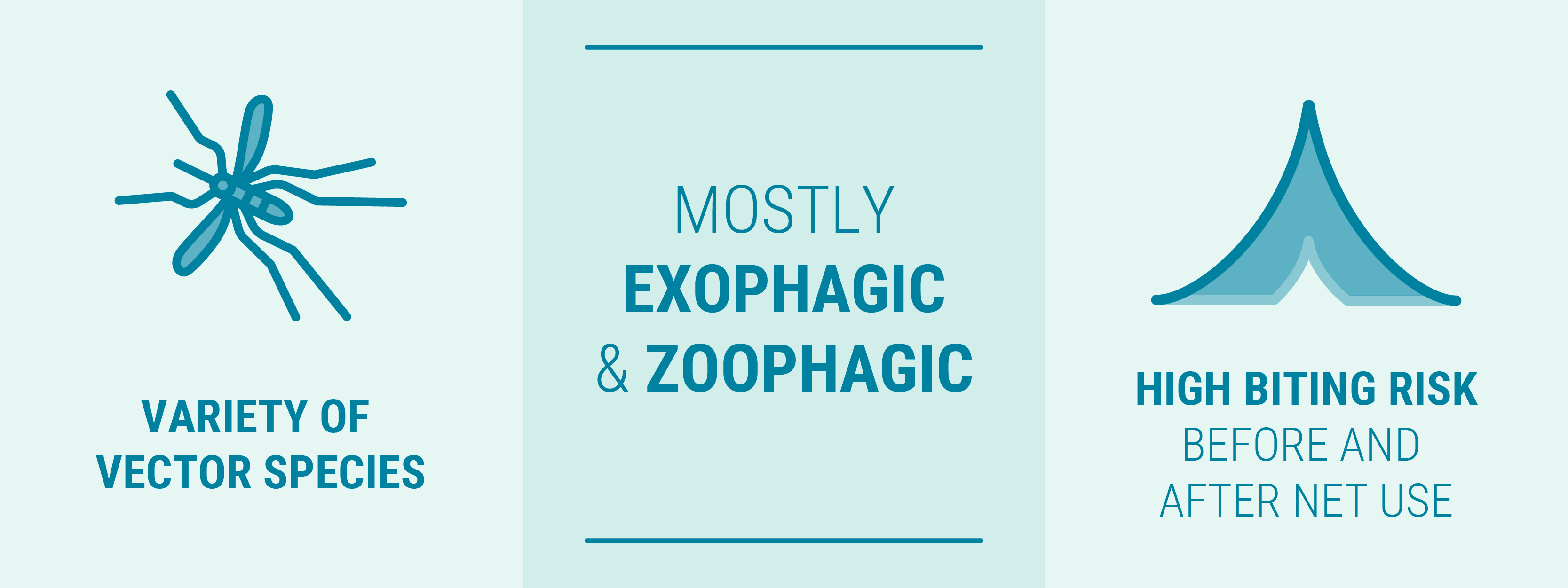
Mosquitoes fed before people went to bed in the evenings and after they woke up in the mornings.
Mosquitoes displayed preference for outdoor feeding (exophagy) and animal feeding (zoophily). By remaining outdoors and feeding on animals, mosquitoes escaped contact with IRS and LLINs.
Higher mosquito abundance existed in forested areas, which is also where LLINs were used less frequently or could not be used.

Research uptake objectives
The research will be used to inform policy, to educate local populations, and to develop simple, cost-effective protocols and tools that can be used locally and more widely by partner agencies across different ecological and epidemiological settings.
International meetings attended
Presentations were given at the following international meetings:
“Residual malaria transmission dynamics varies across the Greater Mekong Subregion despite high coverage of LLINs” – by Jeffrey Hii, American Society Tropical Medicine & Hygiene Symposium; SESSION 168 - Why is Malaria Transmission Persisting in Some Contexts Despite High Coverage of Vector Control Tools, Such as LLINs and IRS? Results From Recent Studies Across Three WHO Regions, New Orleans, Nov 1, 2018
“Vector control at the cross-roads in Asia-Pacific Region: public health entomology and residual malaria transmission” – by Jeffrey Hii, First Malaria World Congress, Melbourne, 1 - 5 July 2018.
“How much Residual Transmission in Greater Mekong Subregion: Thailand & Viet Nam” – Jeffrey Hii, Asia-Pacific Malaria Elimination Network Vector Control Working Group/Mekong Outdoor Malaria Transmission Network 2018 Meeting, Bangkok, 3-5 September 2018
One of his recommendations was to explore personal protection methods that are appropriate within these local areas. He also suggested investigating the durability and ease of use of protection products, as well as those that require minimal behaviour change and communication. The study also highlighted the need for a more holistic definition of RMT, as net use is often overestimated and does not consider people outside of the household, or lower LLIN coverage in farm huts and forest areas.
The meeting led to several important and shared decisions, including an agreement among APMEN members to initiate a multi-country proof of concept study on vector control tools to address outdoor transmission. View more details about the objectives, expected outputs and the agenda of the meeting here.











.png?sfvrsn=95bedc5_1)