
Understanding human, parasite, vector and environmental interactions in Papua New Guinea
Overview
Why this project?
The malaria parasite is transmitted by more than 16 overlapping Anopheles mosquito species adapted to distinct ecologies.
The epidemiology of malaria in the country and consequently, its control are complex and challenging.
The aim
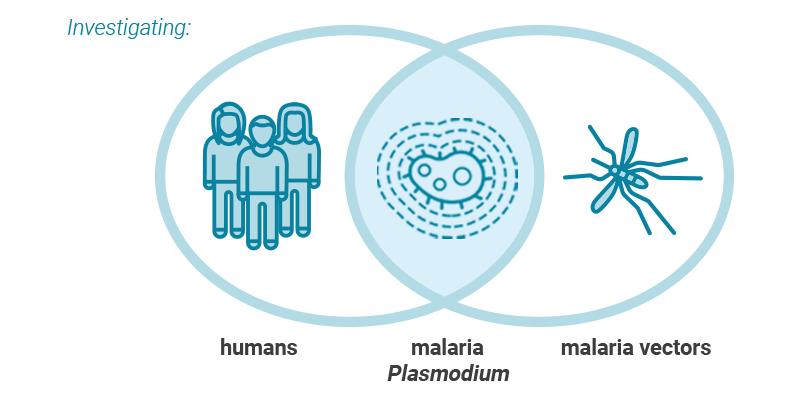
To investigate the prevalence of ongoing malaria transmission and to determine how humans, vectors and their interactions influence human infection by malaria in two sites in Papua New Guinea.
The research sites
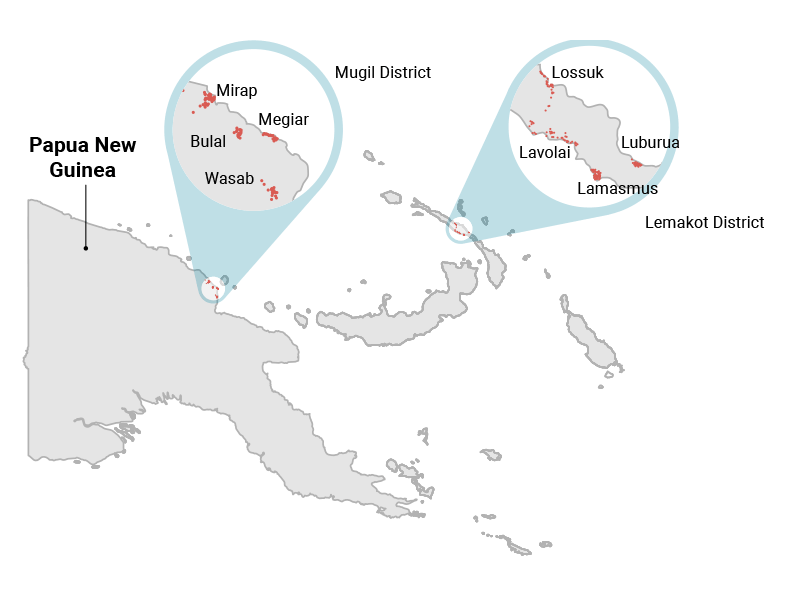
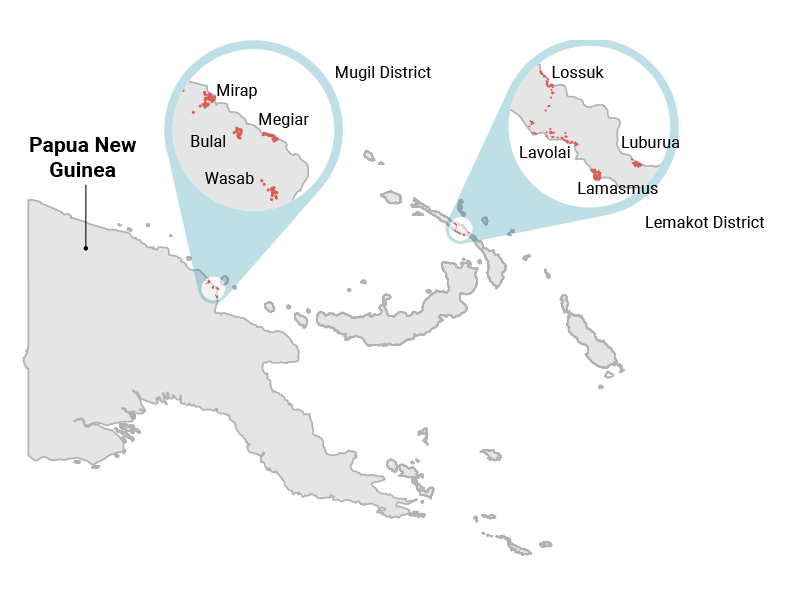
Four villages (Megiar, Mirap, Bulal, Wasab) in the Mugil District, Madang Province
Four villages (Lossuk, Luburua, Lavolai, Lamusmus) in the Lemakot District, New Ireland Province
Research Sites
Mugil District (Madang Province)
Surveys, interviews and sampling were conducted at two coastal villages (Megiar and Mirap) and two inland villages (Bulal and Wasab) in the Mugil district on the north coast of PNG. The inland villages have a wider diversity of vector species, while the coastal villages are dominated by Anopheles farauti. The district has shown consistently high and steady rates of malaria transmission over time. Control efforts have become increasingly successful in the area, although prevalence of some Plasmodium species has been more effectively reduced than others.
Lemakot District (New Ireland Province)
Two villages on the east coast (Lossuk and Luburua) and on the west coast (Lavolai and Lamusmus) were sampled in this district. Lossuk and Luburua are positioned on the beaches and extend a few kilometres into patches of sago swamps, while Lavolai and Lamusmus are further inland from the beaches. The east coast villages also have rivers and streams running either through them or along the edges. Transmission rates and origin in this area remain uncertain but some evidence shows that certain population groups, such as teenage girls, are more susceptible to infection. The prevalence of malaria has dropped from more than 80% to 25% between two original distribution studies in the district (last in 2013).
Research Components
Epidemiological Component
Objective
To investigate and map the prevalence and distribution of malaria infection, and thereby present an overview of the magnitude of ongoing malaria transmission.
Methodology
- Household and individual interviews were conducted at each village (50%-80% of households) using surveys developed with Open Data Kit (ODK). These interviews collected census and GPS data for each household, information on malaria intervention practices, ownership of long-lasting insecticidal nets (LLINs), history of febrile illness and treatment seeking for recent febrile illnesses. Finger prick blood samples were also collected and screened for malaria.
In the Lemakot District, adult mosquito surveys were also conducted at twelve to sixteen households where larvae were found in preliminary studies.
Clinical surveillance systems were established within health facilities at study sites in Mugil District, where febrile patients were screened and tested for malaria. This surveillance has been operating since August 2016. Demographic data and residence location were recorded for each patient and used to create prevalence maps.
Sociological Component
Objective
To identify behaviours that could make different demographic groups within the population more susceptible to ongoing malaria transmission.
Methodology
- In separate groups of men and women, in-depth interviews (IDIs) and focal group discussions (FGDs) were used to discuss day-to-day activities, the amount of time spent outdoors at night/in the early morning and sleeping times. The presence of different malarial hosts and human perceptions of mosquito biting were also discussed.
Areas that are frequently visited and movements between potential areas of high transmission risk in the village and in the surrounding area were also recorded, identified on a map and linked to particular times of the day.
Entomological Component
Objective
To investigate the breeding sites and ecology of local vector populations and their transmission potential. This data was used to identify possible transmission hotspots within each village.
Methodology
- Larval and adult sampling was used to determine the breeding habitat types of the different Anopheles species and to identify transmission hotspots by correlating larval distributions with those of human-biting adult mosquitoes.
Potential breeding grounds for Anopheles mosquitoes were inspected within and on the outskirts of each village. The position of sites with Anopheles larvae was recorded and larvae were collected.
Two to four weeks later, adult mosquitoes were sampled at the breeding sites using human landing catches (HLC) and barrier screens (BS). Using HLC, collection took place both indoors and outdoors for two nights (12-hour period) at each location. Using BS, four screens were set up at each village and adult mosquitoes were collected over 12 hours.
At villages in Lemakot, adult collections were also carried out (2-12 hours) for four nights at common social areas where villagers meet from the afternoon into the early evening and night (e.g. rivers for bathing, sport fields or churches).
Collected larvae and adults were counted and identified to species. This data was used to compare the potential for malaria transmission between coastal and inland villages.
Meteorological Component
Research Components
Research uptake objectives
Objectives: This information can be used to direct targeted control intervention methods in the future and to eliminate key transmission sites for ongoing malaria in these areas.
Key audiences
The key audiences for this study are:
- Local villagers at risk of infection
- Partners
Publications and Other Resources
Publications
No publications have been added.
Gallery
Collaborating Partners
Donors
This work is financially and technically supported by TDR, the Special Programme for Research and Training in Tropical Diseases. Technical support is also provided by the World Health Organization Global Malaria Programme.
Partners
The partners involved in the study on ongoing malaria transmission in Papua New Guinea:
- Papua New Guinea Institute of Medical Research (PNGIMR)
- Papua New Guinea Department of Health
- Burnet Institute
- Swiss Tropical and Public Health Institute (Swiss TPH)
- Walter and Eliza Hall Institute of Medical Research
- Case Western Reserve University
- Pasteur Institut
Contact Details
Contact
Principal Investigators: Dr Leanne Robinson and Dr Moses Laman

